“I was very, very upset to be so belittled and overlooked at a place where you should be believed. It’s just messed up,” junior American studies major Grace Newton said. “It makes me so angry thinking about it now. It really just made me f—ing upset.”

Newton visited an urgent care facility in Villanova, Pa., twice during the same month for flu-like symptoms. She had suffered the flu before and realized that the symptoms she was experiencing were too familiar.
During Newton’s first visit, she told the doctor about her back and muscle pain and how she thought she may have the flu. “He looked at me like, ‘Oh, that’s it? Only back pain? Really, that’s what you came in here for?’” The apparent lack of interest and concern from the doctor was discouraging so she decided to leave.
About a week later, Newton was now feeling very tired, lethargic and she had low energy. She decided to try visiting the local doctor again.
After telling the same doctor about her still-present pain and her added fatigue, the doctor again gave her the same, “That’s it?” look. “If you can’t do 50 percent of your normal day-to-day activities, then that’s when we do tests.”
Newton was baffled that the doctor seemed to minimize her symptoms once again and refused to do any tests. She was highly fatigued, her muscles were still aching and she was sick.
The doctor began talking about her history with anxiety and depression and started to blame all of her symptoms on that. He told Newton that she was wrong for not taking antidepressants. “I think it’s just your anxiety and depression and unless you get cleared–” Newton cut him off.
“Cleared?” she said with anger. Newton was shocked that the doctor had the audacity to blame everything on anxiety and depression. She just wanted to feel better.
Newton was now tearing up and visibly upset. “I was the only African-American at that facility,” Newton said. “I could hear through the walls that he was talking to other patients normally, making jokes and having good conversation. But when he got to me, he was always rude, condescending and did not believe me.”
Newton knew that she was in a wealthy area, but she has top-of-the-line insurance. She did not understand why the doctor treated other patients with more care.
This story is a reoccurring tale for people of color across the United States as they often aren’t believed in the medical field when something is physically wrong. “Black women and men, sometimes when they go to see the doctor, they don’t get the same care because doctors don’t ask the same questions,” Dr. Vivian Smith, associate professor of criminology, said.
Doctors may not be asking the same questions, or vice versa, because they may not be relating to one other. In these cases, doctors are not relating to certain patients in the same way that they would relate to patients who look like them.
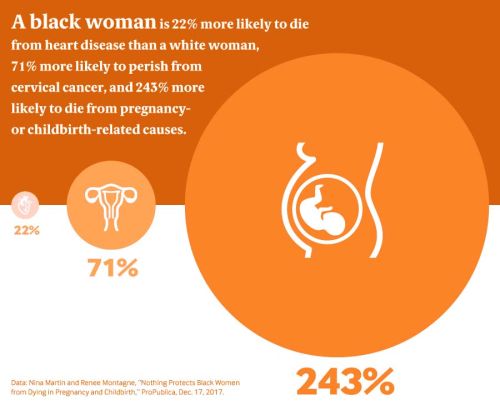
The lack of rapport does not come about because of overt aggression. Rather, smaller mannerisms may lead to patients not feeling understood by doctors. This lack of understanding may result in worse care. “Black women have an increasing risk of heart disease and black men have an increasing risk of prostate cancer because they don’t feel comfortable,” Smith said.
Ms. Ellis, a 50-year-old former custodian who participated in research for an article in the Journal of Black Studies, relates to this lack of understanding. She told the researchers, “I see a lot of white patients come through there and it seems like they [the doctors] listen to them a lot more; they understand them a lot more as opposed to me telling them how I feel and it’s like it’s blowed over.”
After walking out of the same urgent care facility for the second time, Newton was overwhelmed. “In the health care system… where it’s regarding someone’s health, there should not be f—ing discrimination, bias and prejudice,” Newton said. “You are playing with someone’s life.”
Not only did Newton feel that the doctor just downplayed her symptoms once again but the facility also overcharged her. Now she was hyperventilating and crying in the parking lot.
“I was crying in my car and had to call my mom because I didn’t know what to do about everything,” Newton said. “I was so upset because the doctor did not care about how I was feeling. My mom couldn’t even understand me on the phone.”
Newton later calmed down, fixed the overcharge error and vowed to never return to that medical facility ever again.
“It’s a sad state because at the end of the day, you want to think that in those fields that people don’t see color or gender but they do,” Smith said. It is very important to be aware that this is happening. It really does happen, as Newton’s experience shows.
There is a growing awareness that people of different races and backgrounds need to become conscious of the micro-aggressions or implicit acts of bias that they may be putting forth. The doctor may not be aware of his or her own bias. “It doesn’t necessarily have to be a conscious bias. It can be unconscious,” Smith said.
Dr. Ross, Lypson and Kumagai, authors of “Using Illness Narratives to Explore African American Perspectives of Racial Discrimination in Health Care,” in the Journal of Black Studies explain how race-based disparities in the health care system can be unconscious. “Mr. King suggested that he believed the health care system had simply developed a pattern of racist behavior over a period of time and [was] simply doing what they’ve become accustomed to doing — never thinking in their own mind that they handle different people differently,” Ross, Lypson and Kumagai wrote.
This is what is known as implicit bias. A document from the White House Office of Science and Technology explains this term. “Implicit bias manifests in expectations or assumptions that influence their judgements about physical or social characteristics dictated by stereotypes that are based on a person’s race, gender, age, or ethnicity.”
The document further explains that the behaviors resulting from implicit bias can reduce the quality of work, while also being unjust and destructive.
Dr. Ross, Lypson and Kumagai gathered from their data in the Journal of Black Studies that not all of the participants believed that their quality of care was worse because of their race.
However, many did believe that it was still influenced by their race. “Ultimately, all participants experienced encounters in which they reported that health care providers exhibited an overall lack of concern for addressing their health needs and caused them to feel undervalued and unwanted.”
The American Academy of Family Physicians is aware of this possibility in their work environment and they strongly urge their family physicians to explore their own implicit biases.
By exploring their biases, they are bringing self-awareness to their unconscious decisions and how it may negatively affect the communities that they serve. The AAFP also has a PowerPoint posted to the end of their company policy page that educates and addresses the issues of implicit bias in the health care system.
Organizations like the American Academy of Family Physicians are taking the lead in their field to educate health care professionals about implicit bias. The first step to conquering implicit bias and race-based disparities in the health care system is awareness.
Newton hopes that by telling her story readers will realize that you may not always be aware of your own bias and that self-reflection is essential for a healthy environment. Race-based disparities in the health care system are real and are happening today.